Table of Contents
Sterile Surgical Drapes: Unveiling Potential Risks and Complications Introduction
In the crucible of surgical procedures, the significance of sterile surgical drapes is undisputed. Acting as the silent sentinels of the operating theatre, these drapes carry the weighty responsibility of securing sterility and facilitating a contamination-free surgical environment. Yet, every coin has two sides, and so does the sterile surgical drape. While it plays a crucial role in mitigating infection risks, it also harbors potential hazards that can prove counterproductive to its primary mission. This article ventures into the lesser-explored territory of risks and complications associated with sterile surgical drapes and offers insights on their effective management.
Sterile Surgical Drapes: A Multifaceted Story
Sterile surgical drapes are widely acknowledged for their critical role in maintaining sterility and minimizing the risk of surgical site infections (SSIs). However, the story of surgical drapes is a layered one. It is not just about creating a barrier between the sterile and non-sterile areas, but it is also about the delicate balance between the benefits they offer and the potential risks they carry. The complexity and the dynamism of this balance are influenced by numerous factors such as the material of the drape, the manner of its use, and the protocol followed for its disposal. By delving into these aspects, one can unravel the full spectrum of possibilities that accompany the use of surgical drapes.
Material-Related Complications:
Surgical drapes are designed to function as a barrier against the transmission of microorganisms during surgical procedures. However, the effectiveness of this barrier function hinges largely on the material of the drape. If the drape is not adequately fluid-resistant, it can allow the penetration of blood, body fluids, or irrigants, jeopardizing the sterile field. Therefore, the selection of a drape with high fluid resistance is pivotal to prevent this complication.
Moreover, certain types of drapes, particularly those made of non-woven synthetic fabrics, can generate lint or dust. While it may appear harmless, this lint can act as a vehicle for the transmission of bacteria in the surgical environment, thereby escalating the risk of SSIs. Thus, choosing low-linting materials and adhering to strict cleanliness standards in the operating room is essential to curtail this risk.
Additionally, although uncommon, there are instances of allergic reactions or skin irritations caused by the materials or adhesives used in surgical drapes. These adverse reactions can lead to discomfort for the patient and potentially interfere with the surgical procedure. Hence, it’s important to know the patient’s allergy history before choosing the appropriate surgical drape.
Misuse or Improper Application:
Another set of complications related to surgical drapes arises from their misuse or improper application. A drape that is not appropriately positioned or secured may shift or slip during the operation, exposing the non-sterile areas. This can result in the breach of sterility and possibly lead to infections.
Moreover, the formation of fluid pools on the surface of the drape is a commonly overlooked problem. These pools of fluid can serve as a reservoir of microorganisms, contributing to contamination. Therefore, careful application and management of surgical drapes are critical to prevent these complications.
Furthermore, the sterility of surgical drapes is guaranteed only until the package is opened. If the drape is not used immediately after opening, or if it is stored improperly after opening, the chances of contamination significantly increase. This highlights the importance of timely and efficient use of surgical drapes.
Disposal-Related Risks:
The lifecycle of a surgical drape does not end at the conclusion of the surgical procedure. Instead, it transitions into another crucial phase – disposal. Incorrect disposal of used surgical drapes can pose significant risks, primarily due to the potential pathogens they may harbor, especially in the case of infectious surgeries. If these drapes are not correctly disposed of, they can contribute to the spread of healthcare-associated infections (HAIs).
Additionally, improper disposal practices can also put healthcare workers at risk of infections or injuries from contaminated drapes. Thus, adherence to correct disposal protocols is a necessity to safeguard both patient and healthcare worker safety.
Another often overlooked aspect is the environmental impact of incorrect disposal practices. The considerable volume of surgical waste, if not appropriately managed, can contribute to environmental pollution and pose challenges for waste management systems. Therefore, the principles of reduce, reuse, and recycle should be integral to the disposal strategy for surgical drapes.
Navigating the Challenges: Steps towards Safe and Effective Use
Understanding the potential risks and complications associated with surgical drapes is the first step towards formulating strategies to mitigate them. This journey of risk mitigation is underscored by a three-pronged approach focusing on material selection, user training, and regulatory compliance.
Material Selection:
Choosing the right material for surgical drapes can significantly reduce the risks associated with fluid penetration and linting. It is essential to opt for high-quality, fluid-resistant materials that comply with the relevant regulatory standards. Besides, the potential for allergic reactions should also be factored into the selection process.
Training and Education:
Ensuring correct application and use of surgical drapes necessitates regular training and education for healthcare professionals. These programs should emphasize the proper positioning and securing of drapes, the immediate use after opening, and correct storage practices to minimize contamination risks.
Compliance with Disposal Guidelines:
Compliance with local regulations and institutional guidelines is not just a good practice but a legal requirement in surgical waste management. These guidelines provide a comprehensive roadmap for the disposal process, from removal and segregation of used drapes to their transportation, treatment, and final disposal. Adherence to these guidelines can effectively curb the infection risks and environmental implications associated with drape disposal.
Conclusion
The sterile surgical drape, an unsung hero of the operating room, serves a vital purpose in the surgical ecosystem. Its role in maintaining sterility and facilitating a contamination-free surgical environment is invaluable. However, it’s essential to be aware of the potential risks and complications associated with these drapes. By understanding these challenges and implementing effective strategies to navigate them, the full potential of sterile surgical drapes can be harnessed. The story of surgical drapes, thus, evolves from a simplistic narrative of sterility into a nuanced dialogue of safety, responsibility, and continuous learning.
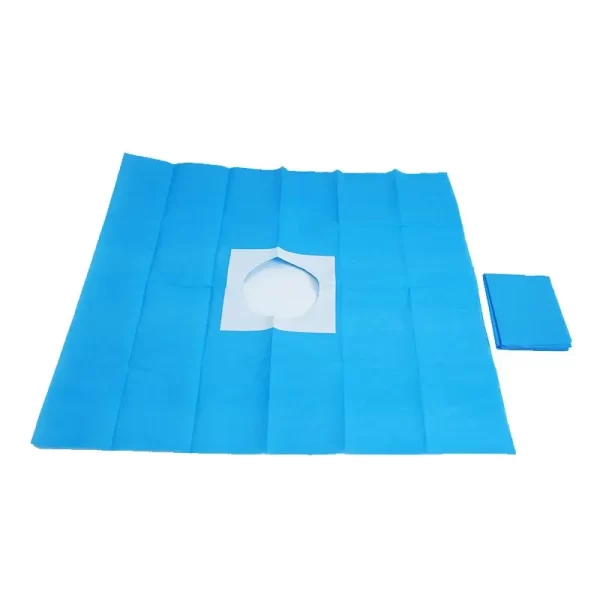
Please visit our website for more product details https://medposnonwoven.com/product/fenestrated-surgical-drape/